
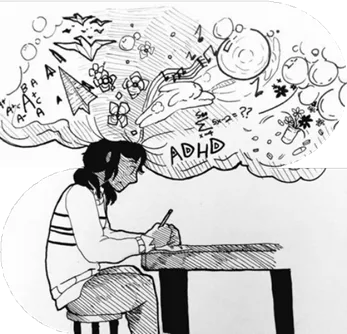
What is ADHD?
Attention-deficit hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorder that might persist across adulthood’s lifespan. The core symptoms of ADHD are difficulties with inattention, impulsivity, and/or motor unrest (i.e., hyperactivity).
Researchers view ADHD as a breakdown in the connectivity, the communication networks, and an immaturity in brain networks. ADHD causes chemical and structural changes in prefrontal cortex (PFC) in brain that is responsible for controlling executive functioning, like planning, decision-making, prioritizing, working toward a goal, and hitting deadlines.
People with ADHD face challenges when it comes to:
- Following through on tasks
- Organizing tasks and activities
- Constantly on the move
- Excessive talking
- Blurting out responses
- Difficulty waiting for a turn
- Interrupting or intruding on others
- Difficulty remaining seated
Reference:
ADDitude. (2021). How the ADHD brain works: The neuroscience behind ADHD symptoms and behaviors such as rejection sensitivity, hyperfocus, emotionality & more (E-book). WebMD LLC. https://www.additudemag.com

Impact on Daily Life
People with ADHD experience difficulties in multiple aspects of their life. These challenges can affect their work, education, and their social relationships. At school or work, they face challenges with time managements because their brain struggles with understanding and conceptualizing the time. They also have problem with following instructions and staying focus on tasks.

Types of ADHD
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), Attention-Deficit/Hyperactivity Disorder (ADHD) is categorized into three main presentations:
- Predominantly Inattentive Presentation
- Predominantly Hyperactive/Impulsive Presentation
- Combined Presentation

1. Predominantly Inattentive Presentation
Predominantly Inattentive Presentation involves a consistent difficulty in sustaining attention, following through on tasks, or staying organized for the past 6 months that is inconsistent with a person’s developmental level and negatively interfere with social and academic/occupational activities.
DSM-s highlighted Common challenges that individuals under 17 years old must have 6 or more symptoms for at least six months and For older adolescents and adults (age 17 and older), need at least five symptoms from the following lists:
✔️Attention to detail
– Making careless mistakes in work, school, or daily activities.
✔️Sustaining focus
– Struggling to stay engaged in conversations, lectures, or reading.
✔️listening
– Seeming distracted, even when spoken to directly.
✔️Following through on tasks
– Starting tasks but quickly losing focus or getting sidetracked.
✔️Organization
– Having trouble keeping track of materials, deadlines, and responsibilities.
✔️Task avoidance
– Finding it hard to start or complete mentally demanding activities.
✔️Losing important items
– Frequently misplacing school or work materials, keys, or phones.
✔️Being easily distracted
– Getting sidetracked by external stimuli or internal thoughts.
✔️Forgetfulness
– Frequently forgetting daily tasks like appointments, chores, or bills.

2. Predominantly Hyperactive/ Impulsive Presentation
In Predominantly Hyperactive/Impulsive Presentation, Children meet the criteria for hyperactivity-impulsivity but not inattention symptoms. They must show Six (or more) of the following symptoms for at least 6 months presistantly in a way that is not is not aligned with their developmental level and that negatively impacts directly on social and academic/occupational activities:
The symptoms are not solely a result of oppositional behaviour , defiance, hostility, or a failure to understand tasks or instructions. For older Adolescents and adults (age 17 and older), at least five symptoms are required:
✔ Fidgeting – You might catch them tapping their hands or feet, or shifting around in their seat, unable to stay still.
✔ Leaving their seat – They may get up when everyone else is supposed to stay seated, like in class, at work, or even during meetings.
✔ Excessive movement – They might run around or climb when it’s not the right place or time, and as adults, this may turn into a feeling of restless energy.
✔ Struggling to be quiet – It’s hard to stay still or quiet during activities that require calmness, like when playing, working, or even relaxing.
✔ Always on the go – Feeling like they’re constantly moving, like they’re powered by a motor—making it tough to just sit and relax for any length of time.
✔ Talking a lot – They may talk more than what’s expected or necessary, often getting caught up in the conversation.
✔ Blurting out – They may interrupt others or finish sentences before they’ve even been completed, always jumping in with something to say.
✔ having trouble waiting – It’s tough to hold back, whether it’s waiting in line or waiting for their turn in a conversation or game.
✔ Interrupting or intruding – They might find themselves cutting into others’ conversations or activities, sometimes using other people’s things without asking.
3.Combined Presentation
This type of ADHD is diagnosed when an individual meets the criteria for both inattention and hyperactivity-impulsivity for a duration of at least six months.
Additional DSM-5 Specifications
✔️ ADHD in Partial Remission:Symptoms were previously met, but now fewer are present, though they stillimpact daily functioning.
✔️ Severity Levels: ADHD can be classified as mild, moderate, or severe, based on the number and intensityof symptoms and their impact on daily life.According to the latest version of the DSM, symptoms must be evident before the age of 12 (rather than anage 7 cut-off for symptom-related impairment in DSM-IV), be pervasive across settings (e.g. home andschool).

Reference:
American Psychiatric Association. (2022).
Diagnostic and statistical manual of mental disorders (5th ed., Text Rev.). American Psychiatric Association Publishing.
Causes of ADHD
ADHD is a complex condition that develops due to a combination of different factors including genetics, brain differences, chemical imbalances, environmental risks, and social factors. While there is no single cause, understanding these factors helps doctors and researchers find better ways to manage and treat ADHD.Here is a list of each major cause in simple terms.
1.Genetics
ADHD often run in families. If a parent or sibling has ADHD, there is a higher chance that a child will also have it. Scientists have found that certain genes related to dopamine, a brain chemical that involved in motivation and attention, are linked to ADHD. Studies on twins also show that identical twins (who have the same DNA) are more likely to both have ADHD compared to fraternal twins. This suggests that genetics plays important roles in ADHD.
2. Brain Structure and Development
Brain scans show that people with ADHD often are different in brain size and development. Some areas, especially the prefrontal cortex, basal ganglia, and cerebellum, are smaller or develop more slowly. These parts of the brain regulate our focus, impulse control, and decision-making explaining why people with ADHD have problem with these skills. Additionally, in some cases, the brain become thin too quickly, which can affect concentration and emotional regulation.
3. Brain Networks and Communication
The brain uses different networks including groups of connected brain areas that help us think and control our behavior. In people who have ADHD, some of these networks don’t function properly:
- The Cognitive-Executive Network (which helps with problem-solving and focus) is weaker in people with ADHD.
- The Cortico-Striatal-Thalamic Network (which helps with motivation and controlling impulses) does not work as efficiently.
- The Default Mode Network (DMN) (which is active when we daydream or relax) is too active in ADHD, making it harder to stay focused.
These differences explain why people with ADHD may have difficulty with paying attention, staying on task, and regulating impulses.
4. Neurotransmitter Imbalance
Neurotransmitters are chemicals that help brain cells communicate. People with ADHD often have dopamine imbalances (DA) and norepinephrine (NE):
- Dopamine (DA): Helps with motivation, reward, and learning. Low dopamine levels can make it harder to stay interested in tasks.
- Norepinephrine (NE): Helps with attention and alertness. When levels are too low, concentration becomes too.
- Serotonin (5-HT), gamma-aminobutyric acid (GABA), and glutamate (Glu) are other brain chemicals that, also affect mood, self-control, and memory, and their imbalance can add to ADHD symptoms.
5. Environmental Factors
Although genetics play a big role in ADHD, external factors can also contribute to ADHD development, including:
- Exposure to toxins (such as lead, pesticides, or pollution) during early childhood.
- Prenatal risks, like smoking, drinking alcohol, or drug use during pregnancy, which can affect the baby’s brain development.
- Premature birth or birth complications, such as lack of oxygen during delivery.
While these factors do not directly cause ADHD, they increase the risk of its development.
6. Psychological and Social Influences
Stressful experiences can worsen symptoms of ADHD while parenting and social environment are not actively correlated how ADHD present.
Factors like:
- Early childhood trauma or neglect
- Growing up in a chaotic or stressful home
- Frequent conflicts with parents or teachers
Creating stressful environment can lead to increased impulsivity, emotional struggles, and difficulty coping with ADHD, meaning how they can severe the symptoms of its development
Reference:
The Neurobiology of ADHD
. (2020). [Monograph]. Retrieved from https://www.teamadhd.com/wpcontent/uploads/2020/05/Neurobiology-Monograph-Digital-Version-1.pdf
How is ADHD Diagnosed ?
ADHD is diagnosed through a detailed evaluation including clinical interviews, standardized rating scales, behavioral observations, and medical history. Since there is no single test for ADHD, diagnosis gather information from various sources, such as parents, teachers, and individuals themselves.
Here’s the main steps of how ADHD is diagnosed:

- Clinical Interviews and History:
Doctors or mental health professionals have detailed interviews to understand the individual’s developmental history, symptoms, and daily challenges. They look for ongoing patterns of inattention, hyperactivity, and impulsivity that have lasted for at least six months and significantly affect daily life.
- DSM-5 Diagnostic Criteria:
The most common criteria for diagnosing ADHD come from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The DSM-5 lists 18 symptoms divided into two categories:
Inattention (e.g., difficulty sustaining attention, forgetfulness, trouble following through on tasks) Hyperactivity/Impulsivity (e.g., excessive fidgeting, interrupting conversations, difficulty waiting for turns)
To be diagnosed, a person must exhibit at least six symptoms from one or both categories (five for adults), and symptoms must
be present in different settings, such as school, work, or home.
- Rating Scales and Questionnaires:
Clinicians often use standardized rating scales to assess ADHD symptoms. These forms are completed by parents, teachers, or the individual themselves to compare behaviors to those of peers. Some commonly used scales include:
Conners Rating Scale
ADHD Rating Scale (ADHD-RS) Vanderbilt Assessment Scales
- Observations in Multiple Settings:
To confirm ADHD and rule out other conditions symptoms must be observed in more than one setting. For example, a child who is inattentive at school but not show at home may not meet the criteria for ADHD.
- Ruling Out Other Conditions:
Since ADHD are coexist to anxiety, depression, learning disabilities, and other mental health disorders, clinicians ensure symptoms are not better explained by another condition.
- Cognitive and Neuropsychological Testing:
In some cases, additional tests assess executive function, working memory, and attention span. While not required for diagnosis, they help understand specific cognitive challenges.
- Adult ADHD Diagnosis:
Adults with suspected ADHD may struggle with organization, poor time management, and impulse control. Since ADHD symptoms change over time, health care providers may focus on reviewing childhood history and assess current difficulties with self-regulation, relationships, and work performance.
Reference:
ADDitude. (2021). How the ADHD brain works: The neuroscience behind ADHD symptoms and behaviors such as rejection sensitivity, hyperfocus, emotionality & more [E-book]. WebMD LLC. https://www.additudemag.com
ADHD: Special Issue on Girls and Women [Magazine]. (2023). Centennial Specialty/A360media Specials.
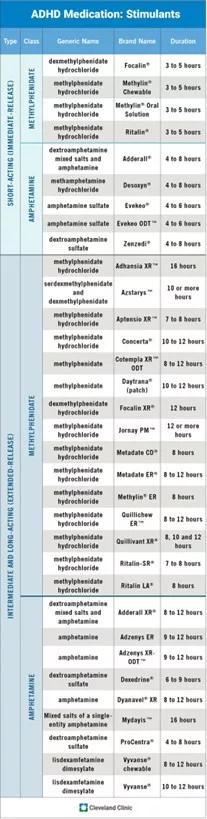
ADHD Medication
Health care providers recommend one or more ADHD medicine depend on type of ADHD and the severity of the symptoms.
There are two main types of medications are Stimulants, non-stimulants
Stimulants:
Stimulants are the first line of medications used for ADHD by increasing the level of neurotransmitters Dopamine and Norepinephrine in the brain to help improve focus, attention, and impulse control. Stimulant medications really depend on the dosage and they often act immediately. These type of medication do not work for everyone and can cause side effects such as insomnia, appetite suppression, and increased heart rate.
Common stimulant medications in the below chart show FDA-approved stimulant ADHD medication.
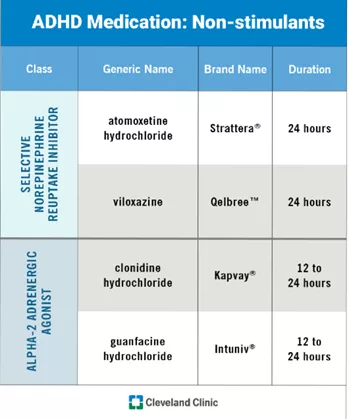
Non Stimulant:
Sometimes stimulant medications can cause intolerable side effects or may not be effective and doctors turn to non-stimulant medication. These medication increase neurotransmitter norepinephrine to help attention and memory. These medications tend to have fewer side effects than stimulants but may still cause drowsiness, dizziness, or stomach issues. Non-stimulants are particularly useful for individuals with ADHD who also have a history of substance abuse, as they have a lower potential for abuse compared to stimulants, The chart shows the most common FDA-approved non-stimulant ADHD medication.
ADHD and Art
What is Art therapy?
Art therapy is a therapeutic approach where people guided by an art therapist to express their feelings, deal with their emotions such as sadness and anxiety to manage their behavior. Art therapist by using human development, psychological theories, and counseling techniques help people to build their self-esteem and reduce anxiety.
Art therapy is a way to help people facing developmental, medical, educational, social, or psychological challenges. Art therapy is worked in mental health, rehabilitation, hospital, and educational settings and also run into individual, couples, family, and group therapy formats. Art therapy has two main branches: art psychotherapy and art as therapy.
Art Psychotherapy uses art to help people explore deep psychological issues and support healing.
Art as Therapy focuses on the creative process using art making to improve emotional and cognitive well-being (Ulman, 1987).
Reference:
Feeney, A. (2024a, March 28). What is art therapy?. Psychology.org. https://www.psychology.org/resources/what-is-art-therapy/
How Art Therapy Helps ADHD?
Art projects typically have a series of ordered steps that work to scaffold the learning process. Following these steps can help children with ADHD improve their attention attention-sequencing skills. For example, first the child focus to choose a project or material. Then, they use their working memory to recall the steps they completed, and practice what to pay attention to ignore distractions – like noises outside – while working on the art project.
Artists also help children practice problem solving and manage frustration tolerance because art often is not predictable as planned. Children with ADHD face challenges while making art like coloring outside a line, or gluing a piece in the wrong spot, by learning how to be flexible and solve problems.
Making art creates a peaceful environment for children to express their thoughts and feelings especially from those who have problems to talk during talk therapy.
Finally, it can build social skills by sharing materials, sharing space, making compliments, or even making suggestions
Reference:
Nelson, S., & Editors, Add. (2022, January 21). Art therapy. ADDitude. https://www.additudemag.com/treatment/art-therapy/? srsltid=AfmBOooY5cf_6AiKYOyCZRHbHZorZKsL_4o9lAr8aKsZCJ0xHpjLNooG
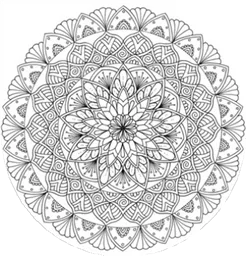
Mandala Art Therapy
Mandela art therapy is an art therapy by coloring circles which are the symbol of wholeness and balance in Hindu and Buddhist symbolism. In this therapy, Mandalas can help children with ADHD create calm energy and improve their focus.
The repetitive patterns and symmetrical forms of a Mandala naturally encourage mindfulness. Coloring inside the lines or designing patterns with details can practice children sustained attention and helps them concentrate in the present moment when faced with distractions.
Mandalas also is a tool for emotional processing. The circular design encourages self-reflection, and children may unconsciously regulate their emotions into their artwork. Creating Mandala can bring inner peace, help reorganize chaotic thoughts, and offer relief from stress or anxiety. Over time, this process can help children become emotionally stronger and better understand their feelings.
This kind of therapy can offer adults to increase their attention span. Mandala coloring can improve executive functioning skills—like attention control, working memory, cognitive flexibility, and problem- solving—making it easier to complete tasks successfully. Babouchkina and Robbin found that adults who color mandalas with circular, symmetrical designs that focus toward the center can experience fewer negative mood symptoms.
Reference:
Singh, C., C, S., & K, J. (2023). Efficacy of mandala coloring intervention on executive functioning and emotional & motivational self- regulation among children with symptoms of attention deficit hyperactivity disorder. Cureus. https://doi.org/10.7759/cureus.46919

ADHD and Music
Using the power of music can bring out emotions and connections. In Music therapy the combination of chords and brain can regulate mood and stress, improve memory and cognition, and even add structure to daily life. Children with ADHD experience benefits from music in terms of rhythm, melody, tempo, and lyrics that help them activate focus, boost organizational skills, incentivize desired behaviors, improve ADHD symptoms, and help you understand hidden thoughts.
Binaural beats, which is created when two tons of slightly different frequencies are played simultaneously, can improve your ability to focus by supporting brain against distractions. Different frequencies entertain different brainwave states that itself improve the ability to focus on tasks.
Reference:
Mt-Bc, P. C. M. (2021, December 13). Rhythm notion: 10 benefits of music for ADHD brains. ADDitude. https://www.additudemag.com/benefits-of- music-adhd/

Calming Music for Better Focus
This music is chosen to help improve focus and reduce distractions — especially helpful for individuals with ADHD or attention difficulties. Feel free to press play and stay a while
Musical Frequencies for People with ADHD
Gamma Waves (30–100 Hz):
When you have difficulty to focus on your doing tasks or to-do lists, this frequency can stimulate your brain into the state of hyper focus. They are powerful and consume a lot of energy so, make sure to use between 1-2 hours a day.
Beta Waves (12 – 30 Hz):
People with ADHD often show lower beta brainwave activity, leading to procrastinate and having problem with initiating tasks.
Frequencies between 15–20 Hz are beneficial for routine tasks or problem-solving

Alpha Waves (8–12 Hz):
If you just want to relax and or needs to do a creative practice, Alpha waves are excellent for you. Alpha brain waves are also great for relaxation, meditation, visualization, and creative tasks.

Theta Waves (4 -8 Hz):
People with ADHD have typically more theta waves, contributing to daydreaming and difficulties with sustained concentration. However, theta waves can be beneficial during short naps to help recharge attention and energy.

Delta Waves (0.5 – 4 Hz):
If you have difficulty in sleeping, then a brainwave frequency that starts in alpha, slows into theta and then to delta can mimic the natural cycle your brain goes through to fall asleep.
To improve your sleep quality, you can get more Delta wave activity which in turn, you can boost your energy during a day.
Reference:
Pearce, K. (2024, September 8). The best music for improving ADHD focus based on science. ADHD Flow State.
Interventions for Teachers

ADHD can cause significant challenges in the classroom, affecting attention, behavior, and academic performance. However, teachers can support students with ADHD by applying effective intervention strategies. Here are lists of strategies that teachers can implement:
Behavioral Interventions
Behavioral interventions focus on modifying classroom environments and behaviors to better support students with ADHD. These interventions are divided into two main categories: antecedent-based (actions taken before behavior occurs) and consequence-based (actions taken after behavior occurs).
Antecedent-Based Strategies:
- Clearly Posting Rules: Classroom rules should be short, clear, positive, and displayed prominently. Teachers should regularly review these rules with students and provide frequent praise to reinforce rule-following behaviors. For students with ADHD, it can be helpful to keep these rules easily visible, such as placing them directly on students’ desks.
- Reducing Task Demands: Assignments should initially match the student’s attention span, with shorter and simplified tasks reducing frustration and disruptive behavior. Teachers can gradually increase the difficulty and length of assignments as students’ attention improves.
- Providing Choices: Offering students a selection of tasks or allowing them to choose the order of activities helps maintain engagement and reduces disruptive behaviors. Giving choices empowers students and makes tasks more appealing, enhancing their involvement and focus.
Consequence-Based Strategies:
Positive Reinforcement: This technique involves giving immediate praise or rewards when students exhibit desirable behaviors, like completing assignments or paying attention. Rewards should be tailored to each student’s interests, varied regularly, and provided promptly after the desired behavior occurs to maximize effectiveness.
Response Cost: In this strategy, students lose previously earned rewards or points as a consequence for negative or disruptive behaviors. Implementing response cost alongside positive reinforcement helps students manage their behavior effectively, enhancing their productivity and classroom conduct.
Time-Out: Time-out involves briefly removing a student from a positive environment following disruptive behavior. It should be used sparingly and combined with positive reinforcement, ensuring the classroom remains a desirable environment for the student.
Self-Management Techniques
Students are taught to assess and monitor their own behavior and performance using simple rating scales. Initially, their self-assessments are compared with teacher evaluations, and students are rewarded based on their accuracy. Over time, students learn to independently regulate their behavior, boosting self-awareness and accountability.
Academic Interventions
While behavioral and medication interventions reduce ADHD symptoms and improve classroom behavior, direct academic interventions are essential. Techniques include direct teacher instruction on specific skills, computer-assisted learning programs, and peer tutoring, all aimed at boosting academic skills and engagement.
Reference:
Kreider, C. M., Medina, S., & Slamka, M. R. (2019). Strategies for coping with time-related and productivity challenges of young people with learning disabilities and attention-deficit/hyperactivity disorder. Children, 6(2), 28. https://doi.org/10.3390/children6020028
Caffeine and ADHD
Moderate caffeine consumption is generally considered safe for some people, while too much caffeine intake can cause various side effects, including nervousness, anxiety, rapid heartbeat, upset stomach, restlessness, migraines, sleeplessness, and muscle tremors.
How does caffeine affect ADHD?
The impact of caffeine on ADHD symptoms is still unclear. Some experts find that caffeine helps improve focus and concentration, while others may experience increased anxiety. Studies suggest that light to moderate caffeine use may benefit some people with ADHD, but its effects are inconsistent and it is not as effective as medication.
The Benefit of Caffeine Consumption
Caffeine can help kids with ADHD pay attention by increasing dopamine levels in the brain by supporting access to executive function skills. For some kids with ADHD, caffeine can have a calming effect by reducing hyperactivity. It can also regulate mood by releasing feel-good chemicals like serotonin.
The Side Effects of Caffeine Consumption
It is essential to be aware of its side effects, especially for people with ADHD. People with ADHD often struggle with sleep problems, and caffeine’s stimulating effects can worsen make sleep problems and ADHD symptoms and harder to manage. Another side effect is anxiety.
People who have ADHD are already prone to anxiety and excessive caffeine intake can increase restlessness, and nervousness.
The Science Behind Coffee and ADHD
To understand the effect of coffee and ADHD, it’s essential to delve into the science behind the relationship between caffeine and brain. Caffeine is a stimulant that block adenosine receptors in the brain. Adenosine is a neurotransmitter that promotes sleep and suppresses arousal. By blocking these receptors, caffeine increases alertness and reduces fatigue.
However, the relationship between caffeine and ADHD is more complex than simple stimulation.
Caffeine also releases dopamine which is responsible for our attention, motivation, and reward-seeking behavior. This interaction between caffeine and dopamine is key to understanding its potential impact on ADHD symptoms. Caffeine consumption may lead to improved focus, increased alertness, and better impulse control, although the effects differently from person to person.
Reference:
Vath, C. (2024, December 3). The truth about caffeine and ADHD. ADDitude. https://www.additudemag.com/adhd-caffeine-treatment/? srsltid=AfmBOor0TCFodGMpdt5JRtrJbWoHViGUlDAWutY6vjxcGCN9BN_awhAY

Hi, I’m Saqhar — I hold a Master’s degree in Special Education, and somewhere along the way, I found a deep passion for ADHD. What started as a simple interest during my studies turned into a commitment to better understanding and supporting individuals with ADHD in real and practical ways.
This website is my way of sharing what I’ve learned — a space for tools, tips, and support, whether you’re living with ADHD, teaching students with ADHD, or supporting a child at home.
My goal is to make information about ADHD more accessible, relatable, and empowering for individuals, families, and educators.






